Symptoms can seem to appear suddenly and include: breast or chest tenderness or swelling on one or both sides, warmth of an area of the breast(s) or chest to the touch, thickening of breast or chest tissue or a lump, pain or a burning sensation continuously or while feeding the baby, redness of some of the skin on the breast(s) or chest, oftentimes in a wedge-shaped pattern, general malaise feeling (feeling like you have the flu), chills, body aches and a fever of 101F (38.3 C) or greater.
Read moreIs It Possible to Relactate?
Your first step is to work with an IBCLC! You can go on Facebook and other social media groups and ask for advice, but you will not be getting an individualized clinical assessment of your own unique situation, so the recommendations you get will not be targeted and in some cases may be harmful.
Read moreBreastfeeding or Chestfeeding in the Early Days: What You Really Need to Know!
After much effort, we have finally started to really inform pregnant people about their labor and birth options. We have included the partner and educated families about the value of having a professional birth attendant like a doula. Pregnant people know which classes to take, what questions to ask, which comfort measures to use. Though we still face abysmal rates of unnecessary medical interventions, there is definitely more access to education and families are better prepared for labor and birth. But where we are still failing is in adequately preparing parents for the newborn phase and especially for normal infant feeding and normal newborn behaviors.
As a private practice IBCLC, I consistently hear from lactating parents during the initial breastfeeding assessment: “I was never told any of this. Why didn’t anyone tell us any of this information?” This even coming from families that took group breastfeeding classes.
The First 24 Hours After Birth
Babies, when born without medicalized interventions, are very alert in the first hour after the birth. This alert state is designed to help babies latch after the birth to initiate the process of signaling to the birth parent’s body that they need nutrients, calories and hydration. After this first hour babies can become very sleepy and can be difficult to rouse over a period of up to the next 24 hours after the birth. This is because, just like birth parents, babies go through a lot of work and energy expenditure during the labor and birth stages.
It is essential that babies be allowed uninterrupted access to the birth parent in the two hours after the birth. I believe that two hours, not one, is essential because of the fact that in the United States birth is highly medicalized and babies need more time to be able to recover from the birth experience and be able to initiate imprinting on the birth parent. During this time having baby skin to skin with the lactating parent, in a calm environment, will allow for hormonal imprinting for the dyad (baby and parent) that will help encourage the process of milk production. In these early moments after birth and especially through the first three days of life, babies need very frequent, small feedings.
Despite the widespread of misinformation, there is, in fact, milk PRESENT AT BIRTH!!! Colostrum IS milk! We need to stop using misleading phrases like “your milk has not come in yet” or “when your milk comes in.” Pregnant people start producing milk, in the form of colostrum, some time around 16 to 20 weeks gestation. This precious first milk is highly concentrated in its protein and other nutritional content, as well as, in its immunological properties. Because of this high concentration of the nutrient content, babies only require small amounts of our first milk. In the first 24 hours post birth, again despite popular misinformation, babies typically only require about 8-10 MLs (about a teaspoon) per feed, depending on the baby’s weight and individual metabolism.
Since baby’s stomach is so very small in size and because human milk is the most perfectly designed food for human digestion, the need for feeds will be quite FREQUENT! In addition, because of the fact that babies can be extra sleepy in the first 24 hours after the birth, you can expect that your baby will be more alert and a lot hungrier on day two. This is a time where baby’s cumulative hunger, from extra long naps and likely ineffective milk transfer on day one, will lead baby to be quite hungry on day two when baby will work hard to catch up.
Day Two After Birth
If baby experienced a highly medicalized birth, it may be that baby may still be recovering on day two and will really start to more actively catch up on feeds on day three. On day two, babies require about 10-12 MLs of milk, as opposed to the 2 ounces typically recommended by MANY healthcare providers in the hospital environment. Because the feeds continue to be small, you can expect the frequency of feedings to be between 8 to, some times, up to 14 feeds per 24 hour period. Babies feed to satiate hunger, to hydrate, and to soothe.
Normal Infant Weight Loss
It is normal for babies to lose about 5 to 7 percent of their birth weight in the first two to four days of life. Some babies will lose as much as 9 to 10 percent of their birth weight. This is NORMAL because the baby passes meconium and urine and is transferring very small amounts and in some case not transferring effectively yet! Let’s all remember that breast or chest feeding is a SKILL, after all. All skills require repetition in order to achieve competency! During this time of normal weight loss it is important that you keep a close eye on baby’s output (the number of urine and poop diapers baby produces per day). You also want weight loss to stop by day four after the birth.
What is important to note is that babies who have experienced a medicalized birth, where the birth parent has received intravenous fluids, can pass meconium and urinate in the first 24 hours as a result of this excess fluid. You want to pay closer attention to baby’s diaper output from day two and beyond. An easy way to remember how to monitor output the first five days of your baby’s life is to expect a number of urine and poop diapers (separately) that is equal to the baby’s age; for example one urine and one poop diaper on day one, two of each on day two, three of each on day three and so on until about day five; after which time each baby will vary depending on their individual caloric needs and intake and should average about 5 to 6 urine diapers and about 4-6 poop diapers per day. Remember these are averages so your baby may be okay with slightly less or more output. This is why it is a good idea to have an early assessment with a highly qualified and experienced International Board Certified Lactation Consultant (IBCLC), who will offer the highest level of clinical lactation expertise.
Day Three, When Things Can Get Really Hard
Day three after birth, whether you are already home with baby after a vaginal delivery or you’re still in the hospital after a cesarean birth, can be a time of a lot of stress. At this point, baby is REALLY HUNGRY and working hard to catch up on caloric intake. Babies can really cluster feed (feed with frequency of as much as every 45 to 60 minutes) for a period of several hours. Baby is not only trying to get more hydration and calories in but also signaling your body to complete the transition from small amounts of milk production in the form of colostrum to larger amounts of mature milk. When your baby cluster feeds your body is alerted that your milk production has to increase to meet your baby’s growing needs. Day three, if you are home, can also feel quite scary because now you and your partner, if you have one, will be fully responsible for your baby’s care without the support of healthcare providers trained in normal newborn behaviors. However, it is important to know that you are CAPABLE of providing optimal, nurturing care for your baby without healthcare experts. You and your baby will quickly learn to communicate especially if you do all of the care for your baby, with the support of others to take care of you and any household chores. The more time you spend with your baby the quicker you will learn your baby’s unique “language.”
Because babies can cluster feed on day three of life and they are likely still experiencing some weight loss, it is very common for pediatricians to suggest you supplement, typically with artificial infant milk. It is important for you to understand that if your baby has lost 10 percent or more of their birth weight and or your baby is showing signs of dehydration (low urine output and or crystals in the urine) that you MUST in fact ensure that your baby gets more milk volume. More often than not, you can provide supplemental human milk feedings by a combination of either hand expressing and or hand expressing and pumping after breastfeeds to collect additional milk to use to feed baby extra calories and achieve adequate hydration. Because you want to make sure that you do not inadvertently cause over stimulation that can lead to over production, it is important to work closely with an experienced IBCLC to ensure an optimal infant feeding and milk production plan. For more information on my recommendations for infant feeding and milk production during the hospital stay or in the first 2 to 3 days after birth, you can read my post Human Milk for Human Babies!!!! STOP Telling Birth Parents, As A Matter of Routine To NOT Pump After Birth.
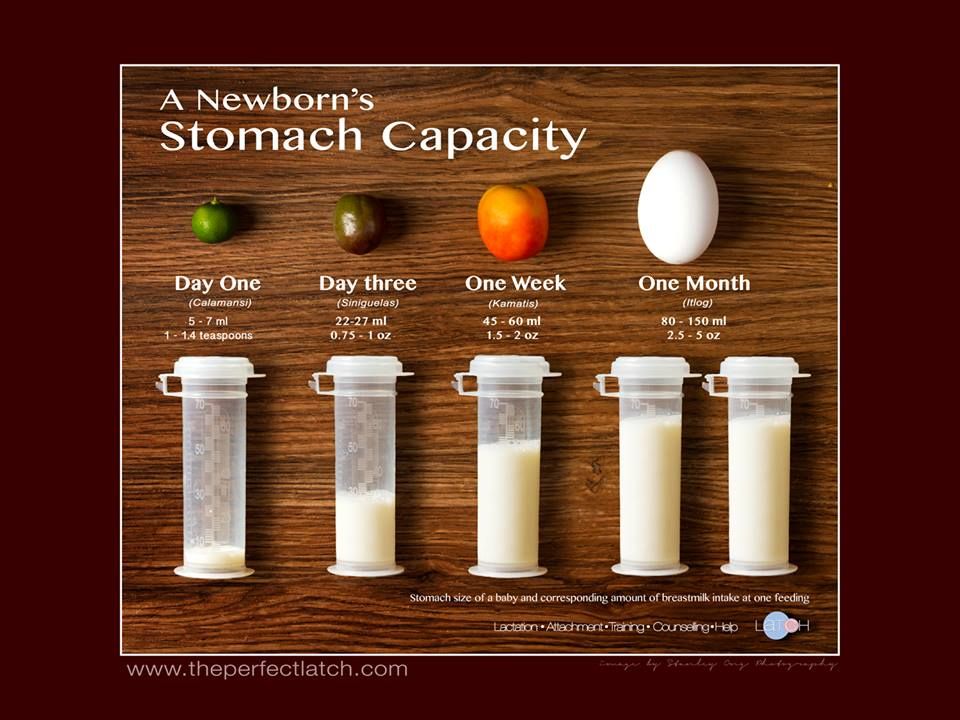
Even just a few more teaspoons of human milk a day, in those early days, can be enough to stop further weight loss and ensure sufficient caloric intake and proper hydration. Most babies do not need the larger quantities of supplementation that many pediatricians often recommend. Your baby’s stomach at birth is about the size of a marble then it grows in the first few days until about day seven where it is about the size of an average apricot and requires about 45 to 60 MLs (or 1.5 to 2 ounces) per feed with still as many as 8 to 12 feeds per day. At around a month of age, your baby’s stomach will be about the size of an average egg and will require about 2.5 to up to 4+ ounces depending on the individual baby, but the average at this age and beyond is more like 2.5 to 3.5 ounces per feed with feeds spread out throughout an entire 24 hour period. The physiological norm for babies is to eat smaller more frequent meals even up to the age of one.
Early Feedings Are Challenging But You CAN Do It!
Breast or chest feeding is definitely challenging, especially in a society like ours that does not value families and does not provide any paid federal family leave to care for our children. With the right information, support and a clear understanding of what is normal infant behavior, you CAN succeed in reaching your infant feeding goals. ASK for and ACCEPT help!!! In the first 4 to 6 weeks post birth, insist on at least a quick weight check appointment at your pediatrician’s office once a week. Keep track of urine and poop output. If your baby needs extra calories, get expert support to create a milk production plan that will provide the extra milk volume your baby is not yet able to get directly at the breast or chest. As long as your baby is not continuing to lose weight, it is okay for your baby to take up to two weeks or a little more to get back up to birth weight. It is normal to have breast fullness and heaviness in the first week or so but you need to get help if your breasts are significantly swollen and or painful. Always get help if the latch is painful beyond the first 20 seconds or so. Nipple damage is never normal so be sure to consult with an IBCLC in the event of any damage.
The first six to, sometimes, eight weeks of breast or chest feeding can be quite challenging and exhausting. You should get help by either hiring an IBCLC, if you can manage it financially, calling your local La Leche League leader or attending a meeting if possible, or if you qualify by getting assistance from an IBCLC at your local WIC program.
Breast is physiologically normal. Fed is required. Informed is BEST!!!!
Breastfeeding/Chestfeeding is NOT just for babies!!!!
The World Health Organization (WHO) recommends exclusive breast or chest feeding for the first 6 months of life after which time babies should be given complimentary foods and continue to be breast or chest fed for up to two years or BEYOND! In the United States, the American Academy of Pediatrics (AAP) mirrors the recommendation of six months of exclusive breast or chest feeding but only recommends duration of up to one year or beyond. As a result of the latter, many birth parents in the United States opt for breast or chest feeding for only six months and those that make it to a year quickly wean upon the first birthday anniversary because they read the AAP's language as stating "up to a year" and do not read the full context of the recommendation: up to a year or BEYOND!
Human Milk
Human milk is not just for newborns and babies. Human milk has been proven to evolve over the period of time that the child continues to consume it. In the second year, between 13-24 months, 448 mLs (slightly more than 15 ounces) of breastmilk has been shown to provide: 29% of energy requirements, 43% of protein requirements, 36% of calcium requirements, 75% of vitamin A requirements, 76% of folate requirements, 94% of vitamin B12 requirements, 60% of vitamin C requirements. (Dewey 2001). We have also found that the fat and energy content of human milk from lactating parents who have been lactating for over one year is greater than that of milk from parents who have been lactating for shorter periods of time (Mandel 2005). It is, therefore, egregious that healthcare professionals, specifically pediatricians in the US, routinely tell parents that human milk after a year has "no nutritional value."
Human milk continues to confer significant nutritional and immunological protections beyond the first year of life. We need to do a much better job of providing accurate, evidence-based information to parents in order to empower them to make informed decisions that best suit their developmental and health goals for their children. Immunity benefits of human milk improve with duration! It takes between two and six years for a child's immune system to fully mature. A number of studies have shown that children that breast or chest feed maintain better health outcomes during the duration of breast or chest feeding. Some studies have also shown that these health benefits may last beyond the duration of breast or chest feeding and may pose greater health benefits long into the individual's life span. (Goldman 1983, Saarenin, U. 1982)
We need to advocate for improved parental support in our society by electing politicians that truly support family values and who will ensure that we have federal protections allowing for significant PAID family leave and lactation services coverage, like other developed nations have. The United States is among just nine countries in the world who do NOT provide any nationwide PAID family leave. There are currently some states that, over the last several years, have legislated paid family leave but we still have no federal protection for paid leave for families.
Breast or Chest Feeding Is MUCH MORE Than Drinking Milk
Breast or chest feeding provides so much more than just human milk consumption and lower morbidity and mortality rates. Feeding at the breast or chest of a parent provides comfort, protection, connection and trust through the unique hormonal imprinting that happens when child and parent connect at the breast or chest. We owe it to our children to provide families with optimal support to ensure that parents are making informed choices about infant and child feeding and that parents receive the appropriate resources to help them reach their goals.
In the United States, there is intense societal pressure on lactating parents to stop breast or chest feeding at a year of age. I experienced this first hand and after a year and a half of relentless scrutiny I weaned my daughter at almost 2.5 years of age. Neither of us were ready and we would have likely naturally weaned a year after my precipitous push to wean her due to the constant intrusions and disapproval. Eleven and a half years later and I still feel pained about the experience and the constant pressure I experienced. Why is it anyone's business when a parent and child end the nursing relationship? What burden does a nursing toddler or child pose on anyone outside of the child parent relationship? The issue, at least partly, stems from the sexualization of breasts in our society. There is NO age or location when breast or chest feeding is inappropriate. Satiating, hydrating and nurturing our children can NEVER be inappropriate. We need to pay closer attention to the language we use because it perpetuates ideas about what is normal and what is not. Calling human milk feeding of a child over the age of one or any age "extended" breast or chest feeding necessitates the assumption that there is an age when nursing stops being appropriate. Normal term breast or chest feeding is what human children do when allowed to naturally evolve in their nursing experience. On average, human children naturally wean, in societies where there is no pressure or intervention to wean, between the ages of 2.5 and 4 years of age, though of course there are some children who will naturally wean earlier and some that when allowed to nurse without constraints or pressure to wean will breast or chest feed for as long as 7 years of age.
Support For Breast Or Chest Feeding Beyond A Year
If you have breast or chest fed your child for ANY duration, I CONGRATULATE you! If you are nursing beyond the first year, I want you to know that only you and your child should determine when it is appropriate to end your nursing relationship. For more support with your normal term nursing experience you can visit kellymom, find a La Leche League meeting for nursing toddlers in the US or else where in the world, visit the Natural Child Project for accurate information on the benefits of normal term breast or chest feeding, or visit kveller or Parenting for encouragement and tips on how to handle the unwarranted societal pressure to wean on someone else's timeline.
For the wonderful mamas in my life that have completed normal term breastfeeding (these parents identify as moms and as breastfeeders): Rachel E., Logan, Kimberleigh, Rachel C., Lexy, Jennifer, Elena, Marah, Tara, Shontay, Ann, Michele L., Mary W. E., Amy, Lisa V., Cynthia, and Lisa S. A.: CONGRATS on your beautiful accomplishment!! For the lovely mamas in my life, and every where, currently nursing your babes past the first year: Karin, Lauren, Jessica, Beth, Jill and Maria: you have my endless love and support any time you need refuge from our often-times punishing world.
“When you hold a child to your breast to nurse, the curve of the little head echoes exactly the curve of the breast it suckles, as though this new person truly mirrors the flesh from which it sprang.” -Diana Gabaldon, Dragonfly in Amber
Human Milk for Human Babies!!!! STOP telling birth parents, as a matter of routine, to NOT pump after birth!
Human Milk for Human Babies
Read moreBlack Babies MATTER!!!
Breastfeeding, because of its important health benefits, is recognized both nationally and globally. In the United States, August is known as Breastfeeding Awareness Month. Every year we celebrate World Breastfeeding Week across the globe from August 1st - 7th. Everyone seems to agree with both of these celebrations and the important health impact these measures deliver.
Black Breastfeeding Week
Six years ago, a group of three black mothers, Kimberleigh Seals Allers, Kiddada Green and Anayah Sangodele-Ayoka, made the crucial decision to use the last week of Breastfeeding Awareness Month, August 25h -31st, to bring specific, targeted awareness to black breastfeeding. Co-founder Anayah Sangodele-Ayoka described Black Breastfeeding Week’s conception to the Huffington Post: “World Breastfeeding Week is typically at the beginning of National Breastfeeding Month (which) had already existed for a few years to be the entirety of the month,” says Sangodele-Ayoka. “So we said, ‘You know what, we don’t need anybody’s permission. We’re just going to take the final week and let everybody know now that’s Black Breastfeeding Week and go from there.’ And that’s how it happened.”
There are some that argue that we do not need to bring special attention to black breastfeeding because "all breastfeeding matters" and "breastfeeding is not about race." Sound familiar? EXACTLY!!! This is pretty much the white privileged outcry, or even at times racism, against #BlackLivesMatter! Only racism or blatant ignorance can lead to the conclusion that Black Breastfeeding Week is redundant or unnecessary.
Black Infant And Maternal Morbidity And Mortality
In the United States, black infants die at a disproportionately HIGHER rate than any other race or ethnicity. Black babies, in our country, are TWO to THREE times more likely to die than white babies. Let that sink in!! For every white baby that dies at least 2-3 black babies die. It is no secret that healthcare disparities as well as the impact of institutionalized racism have a direct impact on the morbidity and mortality of black babies, children, women, and men. Black women die during or after childbirth at THREE times the rate that white women die. These statistics apply across socio-economic backgrounds.
Serena Williams, who undoubtedly has unlimited resources and access to the best care available, almost died after childbirth because of the inherent racism in our healthcare system. Studies have shown that healthcare providers do NOT listen to women and they especially do NOT listen to black women. Had Serena not been a strong, knowledgeable advocate for herself the story would have likely ended tragically.
Black women face unique cultural barriers to breastfeeding. We can NOT ignore the impact that slavery, YES slavery, had on black women and how they see and relate to their bodies. In addition, the rapidly growing field of epigenetics clearly shows us that our sustained history of racism in the US does cause transgenerational genetic change that adversely impacts health outcomes for people of color, particularly black infants, children, women and men.
Representation Matters!
Another reason we do need Black Breastfeeding Week is that representation does MATTER. We know that cultural and ethnic representation in healthcare facilitates better health outcomes. In fourteen years that I have practiced in maternal child health, in both public health and private practice, serving New Jersey and New York City families, I have only ever met FIVE black International Board Certified Lacation Consultants (IBCLCs), and one of them moved back to her homeland of Kenya. Of the FOUR remaining IBCLCs that I know personally, two are in private practice and the other two work for WIC. The communities around me do not reflect this abysmally low number of IBCLCs. We need to do BETTER to empower black women to become IBCLCs by removing the unique barriers that they face.
I wholeheartedly SUPPORT Black Breastfeeding Week because black babies, black women and black families DO MATTER!!!! To help change a broken system please consider supporting organizations like The Perinatal Health Equity Foundation headed by powerhouse Nastassia Davis, RN, IBCLC, NYC Baby Café, Black Mothers Breastfeeding Association, or Black Women Do Breastfeed, among other important organizations and local efforts to promote awareness about black breastfeeding.
HAPPY Black Breastfeeding Week 2018 #LoveOnTop!!!!